by Cliff Harvey, PhD
The interplay between the health of the gut and skin is well known. In this article, Cliff delves into the research on the gut microbiome and skin conditions.
Key points
- The barrier and immune functions of the gut play a role in skin health
- Differing microbiota skin conditions are seen in those with skin conditions versus controls
- Pre- and probiotics are likely to benefit skin conditions
- Several probiotic strains have demonstrated positive results for skin health in studies, including Bifidobacterium bifidum, B. longum, B. lactis, Lactobacillus acidophilus, L. rhamnosus, L. paracasei, Lactococcus lactis
The connection between gut and skin health has been known for some time. Many conditions of the skin such as psoriasis and eczema result from a combination of factors which include allergy and inflammation and so, both the barrier and immune functions of the gut are important for skin health.
Gut health and acne
Acne is an inflammatory skin condition and for nearly a century the link between the gut, brain, and skin has been suggested.1 More recent research has demonstrated that the microbiome of the skin plays an important role in acne and the skin microbiomes of people with and without acne differ.2
The gut microbiome is also important for this condition, due to the roles of the gut as a barrier and immune modulator, and also due to the effects of emotions and stress on motility in the gut and resultant effects on the microbiome, which further affects immunity and inflammation and increases intestinal permeability, contributing to skin inflammation.2

Case-control studies have shown differences in the microbiomes of people with and without acne. Particularly, Actinobacteria was decreased and Proteobacteria (8.35% in increased in acne patients while Bifidobacterium, Butyricicoccus, Coprobacillus, Lactobacillus, and Allobaculum were all decreased.3
Case-control studies have shown differences in the microbiomes of people with and without acne
Changes in diet had typically been considered to have little effect on acne but clinical experience suggests otherwise. It is now suggested that diets that reduce inflammation and support a healthy microbiome, including those based on natural, unrefined foods and with plenty of gut-supporting fibre and resistant starch, be considered for acne.4

https://www.mdpi.com/1422-0067/18/5/1070
In a randomized open-label study, antibiotic treatment and treatment with a probiotic were comparable for reducing acne over 12 weeks (a combination antibiotic and probiotic resulted in the greatest reductions).

Gut health and eczema
Eczema is a common inflammatory condition of the skin affecting around 1 in 10 people at some point in their lives. It has several subtypes:
- Systemic immune or allergy-related: Atopic dermatitis, dyshidrotic eczema, nummular eczema (also known as discoid eczema)
- Contact allergen related: Contact dermatitis, seborrheic dermatitis (caused by a combination of genetics, hormones, and microbes on the skin)
- Related to trauma (possibly also allergen or immune activity): Neurodermatitis (also known as lichen simplex chronicus)
- Related to metabolic dysfunction (along with co-factors of genetics and immune/inflammatory status): Stasis dermatitis (when poor circulation to the legs causes the veins to swell and leak fluid, causing swelling and skin redness and itch—mostly in older people).
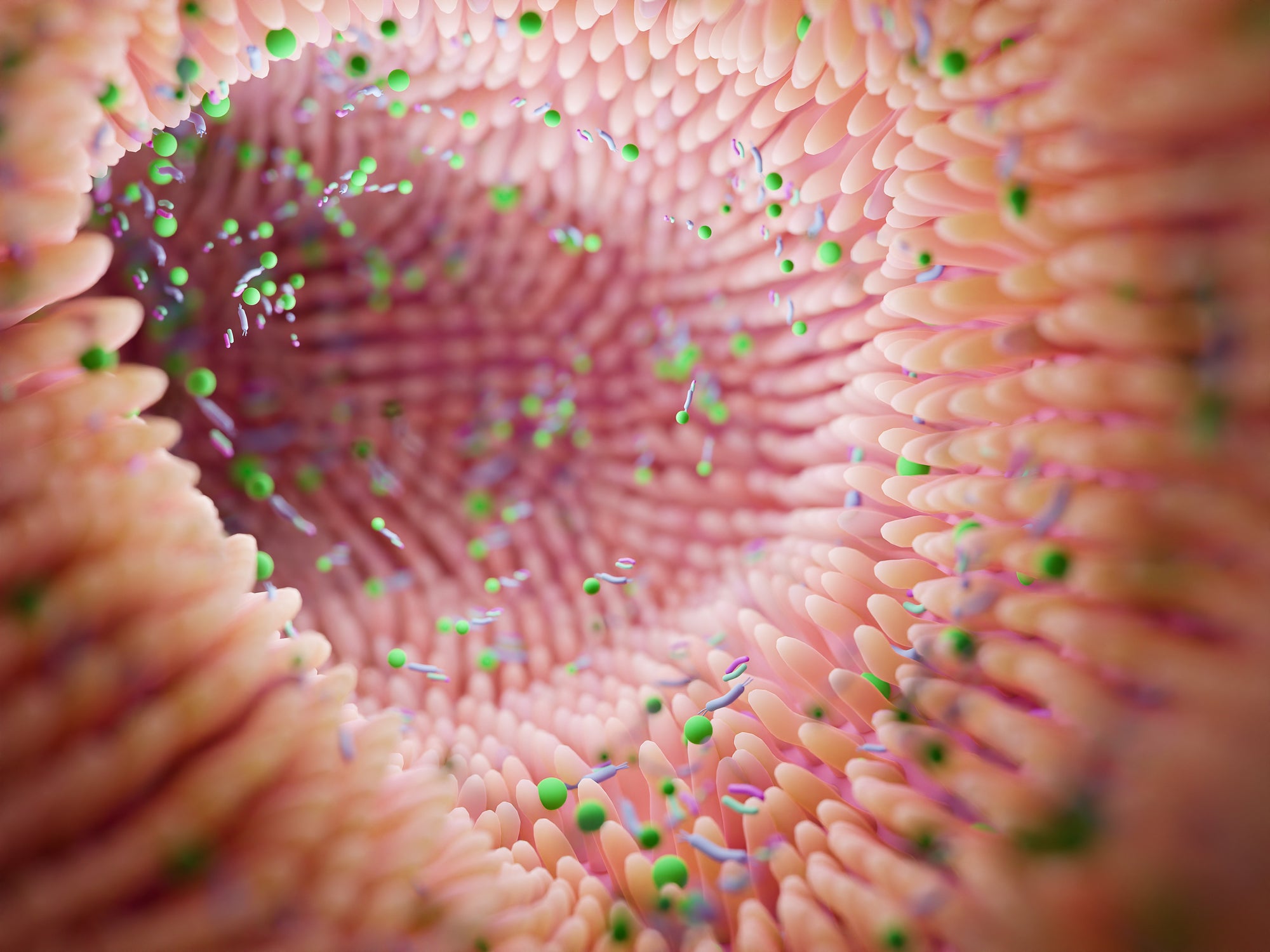
Increasingly, research is demonstrating a link between the gut microbiome and eczema.5 A significant proportion of children who develop food sensitivities go on to develop food allergies and eczema, and these anomalous immune responses are thought to be linked to the gut-immune axis of the body.6
At 1-16 weeks of age, there is lower bacterial diversity in children with atopic and allergic eczema,7-9 and children without eczema have been shown to have up to 56% greater microbial diversity in the intestinal microbiome than those diagnosed with eczema.10, 11 In other research, at 6 months of age, healthy children had 3-fold greater amounts of Bacteroidetes, while microbiota of children suffering from eczema had increased abundance of the Clostridium clusters IV and XIVa, which are typically more abundant in adults.12

Additionally, lower numbers of Ruminococcaceae, Bifidobacterium, Megasphaera, Haemophilus, Streptococcus and Lactobacillus species, and higher levels of Escherichia/Shigella, Veillonella, Faecalibacterium, Lachnospiraceae incertae sedis and Enterobacteriaceae, Bacteroidaceae, Clostridiaceae, Deinococcaceae and E.coli are associated with eczema in children and the sensitization to allergies, and asthma.13-19
Reduced abundance of Ruminococcaceae and Enterobacteriaceae seen in children with eczema (at 1-4 weeks of age) has been associated with increased inflammation (Il-6 and TNF- α ). Mothers whose infants developed IgE‐associated eczema had lower α‐diversity of Bacteroidetes (although this was not seen later in their infants). At 1 year, α‐diversity of Actinobacteria was lower in infants with IgE‐associated eczema compared with controls.20

However, differing species within the same genus could result in quite different outcomes. For example, in children up to 1-year-old, the presence of B. catenulatum at 3 months was associated with a higher risk of developing eczema [1], infants colonised with B. breve up to 3 months had a reduced risk of developing eczema [2] and the presence of B. breve at 3 months was associated with a lower risk of atopic sensitization at 12 months. B. breve colonization patterns were influenced by maternal allergic status, household pets and number of siblings.21 Additionally, breast-fed infants are more likely to harbour Bifidobacterium bifidum [3], while Bifidobacterium pseudocatenulatum was detected more commonly in faeces of non–breast-fed children [4] and children with eczema, but there were no significant associations between clinical measurements and detection of B pseudocatenulatum.22
Several species, such as Faecalibacterium rausnitzii and Ruminococcus gnavus, that are known to be associated with atopy or inflammation, were found to be significantly enriched in infants with eczema. Higher abundance of Akkermansia muciniphila in eczematous infants might reduce the integrity of intestinal barrier function and therefore increase the risk of developing eczema. On the other hand, Bacteroides fragilis and Streptococcus salivarius, which are known for their anti-inflammatory properties, were less abundant in infants with eczema.18
A role for ‘superantigens’?
Certain bacteria carrying ‘superantigens’ might also promote the later development of allergic sensitization and eczema. For example, while the early gut colonization by Staphylococcus aureus was not related to subsequent eczema development, the S. aureus strains that were found to colonize those infants who developed atopic eczema were less likely to carry the gene encoding a ‘superantigen’ (SE lM) and the gene for elastin‐binding protein compared with strains that were isolated from infants who had not developed atopic eczema by 18 months of age.23
Metabolites
Reduced short-chain fatty acids produced by gut bacteria along with succinate, phenylalanine and alanine, and higher glucose, galactose, lactate, and lactose have been found in faecal samples of children who later developed eczema. Supplementation of multi-species probiotics induces higher levels of lactate and short-chain fatty acids, and lower levels of lactose and succinate (compared to placebo) and this might explain some of the protective roles for probiotics on the development of eczema.24
Reduced short-chain fatty acids and higher glucose, galactose, lactate, and lactose have been found in faecal samples of children who later developed eczema.
Probiotics for eczema
There is some debate about the role that probiotics might play in eczema. Overall, systematic reviews of the literature suggest around a 26% reduction in risk for eczema with probiotic supplementation,25 and current evidence supports the use of Lactobacillus strains for the prevention of eczema. Prebiotics have also been shown beneficial for primary prevention of eczema in formula-fed infants with prolonged use greater than 6 months.26 However, results differ between probiotic species.
In a randomized, double‐blind, placebo‐controlled trial, 112 pregnant women with a family history of allergic diseases received a once‐daily supplement, either a mixture of Bifidobacterium bifidum BGN4, B. lactis AD011, and Lactobacillus acidophilus AD031, or placebo, starting 4-8 weeks before delivery and continuing 6 months post-delivery. The prevalence of eczema at 1 year in the probiotic group was significantly lower than in the placebo group (18.2% vs. 40.0%) and the cumulative incidence of eczema during the first 12 months was reduced significantly in probiotic group (36.4% vs. 62.9%). However, there was no significant difference in allergies between the groups.27
The probiotic Lactobacillus rhamnosus (HN001) might also reduce eczema risk. In an analysis of faecal samples from 650 infants, L. rhamnosus HN001, Bifidobacterium animalis lactis HN019 supplementation resulted in a 50% reduced eczema risk in the HN001 probiotic group compared to placebo.28
In a double-blind, placebo-controlled study of (241 mother-infant pairs), mothers with allergic disease and atopic sensitization were randomly assigned to receive Lactobacillus rhamnosus LPR and Bifidobacterium longum BL999 (LPR+BL999), L. paracasei ST11 and B. longum BL999 (ST11+BL999), or placebo, beginning 2 months before delivery and during the first 2 months of breast-feeding. The risk of developing eczema during the first 24 months of life was significantly reduced in infants of mothers receiving probiotics.[5]29
In a double‐blind, randomized, placebo‐controlled trial, a mixture of the probiotics Bifidobacterium bifidum, Bifidobacterium lactis, and Lactococcus lactis (Ecologic® Panda) was administered prenatally and during the first 12 months after the birth of both the mother and child. This resulted in significantly lower rates of eczema at 3 months and lower cumulative eczema over 2 years, along with greater colonisation by Lc.lactis.30
Lactobacillus rhamnosus GG (LGG; 10 billion CFU per day) and 225 mg of inulin supplementation did not appear to reduce the incidence of eczema, asthma, or rhinitis in infants between 0 and 2 years of age.31 Similarly, a trial of Bifidobacterium longum and Lactobacillus rhamnosus supplemented cow’s milk formula did not affect eczema or allergen sensitization in the first year of life in Asian infants at risk of allergic disease.32
Systematic reviews of the literature suggest around a 26% reduction in risk for eczema with probiotic supplementation.
Prebiotics
The faecal microbiota of formula-fed children supplemented prebiotic fibre is closer to that of breastfed children than infants receiving standard formula.33
Other gut-factors that influence the microbiome and eczema34:
Full-term vaginal birth allows for the greatest transference of microbiota to the baby during birth. Breast milk also contains indigestible carbohydrates that encourage the population of the infants gut with health-promoting bacteria,35, 36 and also contains bacteria transported to the mammary glands via the enteromammary pathway.
Attempts have been made to mimic this pre- and probiotic activity of breast milk. Prebiotic supplementation added to formula increases the number of bifidobacteria to a level comparable to breastmilk and reduces the pathogenic bacteria Clostridium dificile.37 Inulin (a prebiotic fibre) has demonstrated efficacy in increasing bifidobacteria in the gut.38
Prebiotic supplementation added to formula increases the number of bifidobacteria to a level comparable to breastmilk.
Gut health and psoriasis
The gut-skin axis is be related to the immune-inflammatory cascade. There is, for example, an increased prevalence of psoriasis and psoriatic arthritis with inflammatory bowel disease.39 The gut microbiota of patients with psoriasis also shows reduced diversity,40 and a distinct ‘signature’ compared to controls.41 There is an increased abundance of Firmicutes and decreased Bacteroidetes with Ruminococcus and Megasphaera (phylum Firmicutes) the top‐two genera abundant in psoriasis,42 while veillonella in faecal microbiota showed a positive relationship with h-CRP in blood.43
The abundance of Akkermansia muciniphila was also significantly reduced in patients with psoriasis and this bacteriais believed to have an important function in the pathogenesis of inflammation, inflammatory bowel diseases and obesity.44
In a case study, a 36-year-old male with plaque psoriasis and irritable bowel syndrome was given 2 faecal microbiota transplants 5 weeks apart. Following the second treatment, his IBS was completely resolved with no adverse reactions observed.46

Probiotics likely to be of benefit to the skin
- Bifidobacterium bifidum
- B. longum
- B. lactis
- Lactobacillus acidophilus
- L. rhamnosus
If you are looking for an easy way to get your daily-dose of probiotics, Digestive Support Protein by Nuzest might be a good choice for you. Digestive Support Protein is European Golden Pea protein blended with probiotics and other gut-friendly ingredients targeted at healthy digestive support. It contains 975 CFU of bacillus coagulans per 25 gram serving.
References
1. Bowe WP, Logan AC. Acne vulgaris, probiotics and the gut-brain-skin axis – back to the future? Gut Pathogens. 2011;3(1):1.
2. Lee YB, Byun EJ, Kim HS. Potential Role of the Microbiome in Acne: A Comprehensive Review. Journal of Clinical Medicine. 2019;8(7):987.
3. Yan H-M, Zhao H-J, Guo D-Y, Zhu P-Q, Zhang C-L, Jiang W. Gut microbiota alterations in moderate to severe acne vulgaris patients. The Journal of Dermatology. 2018;45(10):1166-71.
4. Clark AK, Haas KN, Sivamani RK. Edible Plants and Their Influence on the Gut Microbiome and Acne. International Journal of Molecular Sciences. 2017;18(5):1070.
5. Köberle M, Biedermann T. [Microbiome, atopic eczema and blockade of type 2 immunity]. Der Hautarzt; Zeitschrift fur Dermatologie, Venerologie, und verwandte Gebiete. 2018;69(3):197-203.
6. Marrs T, Flohr C. How do Microbiota Influence the Development and Natural History of Eczema and Food Allergy? The Pediatric Infectious Disease Journal. 2016;35(11):1258-61.
7. Wang M, Karlsson C, Olsson C, Adlerberth I, Wold AE, Strachan DP, et al. Reduced diversity in the early fecal microbiota of infants with atopic eczema. Journal of Allergy and Clinical Immunology. 2008;121(1):129-34.
8. Forno E, Onderdonk AB, McCracken J, Litonjua AA, Laskey D, Delaney ML, et al. Diversity of the gut microbiota and eczema in early life. Clinical and Molecular Allergy. 2008;6(1):11.
9. Abrahamsson TR, Jakobsson HE, Andersson AF, Björkstén B, Engstrand L, Jenmalm MC. Low diversity of the gut microbiota in infants with atopic eczema. Journal of Allergy and Clinical Immunology. 2012;129(2):434-40.e2.
10. Diversity of the Gut Microbiota and Eczema in Infants. D47 NEONATAL AND RARE LUNG DISEASES. p. A5981.
11. Ismail IH, Oppedisano F, Joseph SJ, Boyle RJ, Licciardi PV, Robins-Browne RM, et al. Reduced gut microbial diversity in early life is associated with later development of eczema but not atopy in high-risk infants. Pediatric Allergy and Immunology. 2012;23(7):674-81.
12. Nylund L, Satokari R, Nikkilä J, Rajilić-Stojanović M, Kalliomäki M, Isolauri E, et al. Microarray analysis reveals marked intestinal microbiota aberrancy in infants having eczema compared to healthy children in at-risk for atopic disease. BMC Microbiology. 2013;13(1):12.
13. Tang MF, Sy HY, Kwok JSL, Tam WH, Hon KL, Tung CKC, et al. Eczema susceptibility and composition of faecal microbiota at 4 weeks of age: a pilot study in Chinese infants. British Journal of Dermatology. 2016;174(4):898-900.
14. Zimmermann P, Messina N, Mohn WW, Finlay BB, Curtis N. Association between the intestinal microbiota and allergic sensitization, eczema, and asthma: A systematic review. Journal of Allergy and Clinical Immunology. 2019;143(2):467-85.
15. Zhang Y, Jin S, Wang J, Zhang L, Mu Y, Huang K, et al. Variations in early gut microbiome are associated with childhood eczema. FEMS Microbiology Letters. 2019;366(9).
16. Wang H, Li Y, Feng X, Li Y, Wang W, Qiu C, et al. Dysfunctional gut microbiota and relative co-abundance network in infantile eczema. Gut Pathogens. 2016;8(1):36.
17. Penders J, Stobberingh EE, Thijs C, Adams H, Vink C, Van Ree R, et al. Molecular fingerprinting of the intestinal microbiota of infants in whom atopic eczema was or was not developing. Clinical & Experimental Allergy. 2006;36(12):1602-8.
18. Zheng H, Liang H, Wang Y, Miao M, Shi T, Yang F, et al. Altered Gut Microbiota Composition Associated with Eczema in Infants. PloS one. 2016;11(11):e0166026-e.
19. Mah KW, Björkstén B, Lee BW, van Bever HP, Shek LP, Tan TN, et al. Distinct Pattern of Commensal Gut Microbiota in Toddlers with Eczema. International Archives of Allergy and Immunology. 2006;140(2):157-63.
20. West CE, Rydén P, Lundin D, Engstrand L, Tulic MK, Prescott SL. Gut microbiome and innate immune response patterns in IgE-associated eczema. Clinical & Experimental Allergy. 2015;45(9):1419-29.
21. Ismail IH, Boyle RJ, Licciardi PV, Oppedisano F, Lahtinen S, Robins-Browne RM, et al. Early gut colonization by Bifidobacterium breve and B. catenulatum differentially modulates eczema risk in children at high risk of developing allergic disease. Pediatric Allergy and Immunology. 2016;27(8):838-46.
22. Gore C, Munro K, Lay C, Bibiloni R, Morris J, Woodcock A, et al. Bifidobacterium pseudocatenulatum is associated with atopic eczema: A nested case-control study investigating the fecal microbiota of infants. Journal of Allergy and Clinical Immunology. 2008;121(1):135-40.
23. Nowrouzian FL, Lina G, Hodille E, Lindberg E, Hesselmar B, Saalman R, et al. Superantigens and adhesins of infant gut commensal Staphylococcus aureus strains and association with subsequent development of atopic eczema. British Journal of Dermatology. 2017;176(2):439-45.
24. Kim HK, Rutten NBMM, Vaart IB-vd, Niers LEM, Choi YH, Rijkers GT, et al. Probiotic supplementation influences faecal short chain fatty acids in infants at high risk for eczema. Beneficial Microbes. 2015;6(6):783-90.
25. Mansfield JA, Bergin SW, Cooper JR, Olsen CH. Comparative Probiotic Strain Efficacy in the Prevention of Eczema in Infants and Children: A Systematic Review and Meta-Analysis. Military Medicine. 2014;179(6):580-92.
26. Szari S, Quinn JA. Supporting a Healthy Microbiome for the Primary Prevention of Eczema. Clinic Rev Allerg Immunol. 2019;57(2):286-93.
27. Kim JY, Kwon JH, Ahn SH, Lee SI, Han YS, Choi YO, et al. Effect of probiotic mix (Bifidobacterium bifidum, Bifidobacterium lactis, Lactobacillus acidophilus) in the primary prevention of eczema: a double-blind, randomized, placebo-controlled trial. Pediatric Allergy and Immunology. 2010;21(2p2):e386-e93.
28. Murphy R, Morgan XC, Wang XY, Wickens K, Purdie G, Fitzharris P, et al. Eczema-protective probiotic alters infant gut microbiome functional capacity but not composition: sub-sample analysis from a RCT. Beneficial Microbes. 2019;10(1):5-17.
29. Rautava S, Kainonen E, Salminen S, Isolauri E. Maternal probiotic supplementation during pregnancy and breast-feeding reduces the risk of eczema in the infant. Journal of Allergy and Clinical Immunology. 2012;130(6):1355-60.
30. Niers L, Martín R, Rijkers G, Sengers F, Timmerman H, Van Uden N, et al. The effects of selected probiotic strains on the development of eczema (the PandA study). Allergy. 2009;64(9):1349-58.
31. Cabana MD, McKean M, Caughey AB, Fong L, Lynch S, Wong A, et al. Early Probiotic Supplementation for Eczema and Asthma Prevention: A Randomized Controlled Trial. Pediatrics. 2017;140(3):e20163000.
32. Soh SE, Aw M, Gerez I, Chong YS, Rauff M, Ng YPM, et al. Probiotic supplementation in the first 6 months of life in at risk Asian infants – effects on eczema and atopic sensitization at the age of 1 year. Clinical & Experimental Allergy. 2009;39(4):571-8.
33. Wopereis H, Sim K, Shaw A, Warner JO, Knol J, Kroll JS. Intestinal microbiota in infants at high risk for allergy: Effects of prebiotics and role in eczema development. Journal of Allergy and Clinical Immunology. 2018;141(4):1334-42.e5.
34. Chan CWH, Wong RS, Law PTW, Wong CL, Tsui SKW, Tang WPY, et al. Environmental Factors Associated with Altered Gut Microbiota in Children with Eczema: A Systematic Review. International Journal of Molecular Sciences. 2016;17(7):1147.
35. Jost T, Lacroix C, Braegger C, Chassard C. Impact of human milk bacteria and oligosaccharides on neonatal gut microbiota establishment and gut health. Nutrition reviews. 2015;73(7):426-37.
36. Jost T, Lacroix C, Braegger CP, Rochat F, Chassard C. Vertical mother-neonate transfer of maternal gut bacteria via breastfeeding. Environ Microbiol. 2014;16(9):2891-904.
37. Holscher HD, Faust KL, Czerkies LA, Litov R, Ziegler EE, Lessin H, et al. Effects of prebiotic-containing infant formula on gastrointestinal tolerance and fecal microbiota in a randomized controlled trial. JPEN Journal of Parenteral & Enteral Nutrition. 2012;36(1 Suppl):95S-105s.
38. Holscher HD, Bauer LL, Gourineni V, Pelkman CL, Fahey Jr GC, Swanson KS. Agave Inulin Supplementation Affects the Fecal Microbiota of Healthy Adults Participating in a Randomized, Double-Blind, Placebo-Controlled, Crossover Trial. Journal of Nutrition. 2015;145(9):2025-32.
39. Myers B, Brownstone N, Reddy V, Chan S, Thibodeaux Q, Truong A, et al. The gut microbiome in psoriasis and psoriatic arthritis. Best Practice & Research Clinical Rheumatology. 2020:101494.
40. Hidalgo‐Cantabrana C, Gomez J, Delgado S, Requena‐López S, Queiro‐Silva R, Margolles A, et al. Gut microbiota dysbiosis in a cohort of patients with psoriasis. British Journal of Dermatology. 2019;181(6):1287-95.
41. Codoñer FM, Ramírez-Bosca A, Climent E, Carrión-Gutierrez M, Guerrero M, Pérez-Orquín JM, et al. Gut microbial composition in patients with psoriasis. Scientific Reports. 2018;8(1):3812.
42. Chen YJ, Ho HJ, Tseng CH, Lai ZL, Shieh JJ, Wu CY. Intestinal microbiota profiling and predicted metabolic dysregulation in psoriasis patients. Experimental dermatology. 2018;27(12):1336-43.
43. Huang L, Gao R, Yu N, Zhu Y, Ding Y, Qin H. Dysbiosis of gut microbiota was closely associated with psoriasis. Science China Life Sciences. 2019;62(6):807-15.
44. Tan L, Zhao S, Zhu W, Wu L, Li J, Shen M, et al. The Akkermansia muciniphila is a gut microbiota signature in psoriasis. Experimental dermatology. 2018;27(2):144-9.
45. Castelino M, Tutino M, Moat J, Ijaz U, Parslew R, Al-Sharqi A, et al. AB0115 Comparison of the bacterial stool microbiota in established psoriatic arthritis (PSA) and psoriasis (PSC)-exploratory analysis of pilot data. BMJ Publishing Group Ltd; 2017.
46. Yin G, Li J, Sun Y, Ding X, Zeng J, Zhang T, et al. Fecal microbiota transplantation as a novel therapy for severe psoriasis. Zhonghua nei ke za zhi. 2019;58(10):782-5.
[1] OR adj = 4.5; 95% CI : 1.56–13.05, padj = 0.005
[2] (OR adj = 0.15; 95% CI : 0.05–0.44, padj = 0.00001)
[3] (odds ratio, 5.19; 95% CI, 1.47-18.36; P = .01).
[4] (odds ratio, 5.6; 95% CI, 1.3-24.3; P = .02) eczema, 26%; no eczema, 4%; P = .04
[5] LPR+BL999 (odds ratio [OR], 0.17; 95% CI, 0.08-0.35; P < .001) and ST11+BL999 (OR, 0.16; 95% CI, 0.08-0.35; P < .001).