By: Cliff Harvey PhD
When people talk about the gut, they’re referring to the gastrointestinal system, also known as the digestive system or digestive tract. This system includes the mouth, oesophagus, stomach, and the small and large intestine. It also includes the accessory organs which aid digestion by helping to break down larger particles of food into absorbable particles (i.e. the tongue, salivary glands, pancreas, liver, and gallbladder). Read on to learn all about gut health and some tips to have a healthy gut.
Table of Contents
- What is gut health?
- Why is gut health important?
- Is gut health a fad?
- What is the microbiome?
- What are probiotics?
- What are prebiotics?
- Effects of the gut on health
- The gut-brain link and the effects of gut-health on mental health (and vice versa!)
- Gut health and sleep
- Gut health and skin health
- Can gut health cause hair loss?
- Can gut health affect blood pressure?
- Can gut health cause headaches?
- How does gut health affect hormones?
- Does gut health affect weight loss?
- Gut health, diabetes, and cardiometabolic health
- Cardiovascular health
- Are protein powders good for gut health?
- Are probiotics good for gut health?
- Lifestyle and gut health
- Do sweeteners harm the microbiome?
- Relationship between gut health and overall health
What is gut health?
Having a healthy digestive system, also known as having good gut health, allows us to absorb nutrients optimally and helps to reduce inflammation, support immunity, and even plays a role in helping us to feel better mentally.
Why is gut health important?
Because it’s exposed to the external environment, the digestive system is an external organ by which we absorb the nutrients that make up the body’s structures, chemical messengers, and fuels. Because it’s exposed to the outside environment, it is also a potential site of infection from pathogens (disease-causing microbes) and pollutants in food and water and so, is part of our innate defences against disease and disorder that has an important relationship with the immune system of the body.
Is gut health a fad?
Because the role of the gut is so important for both nourishment and immunity, gut health couldn’t be called a fad. Having a healthy gut is an essential component of wellbeing! However, there can be dubious claims made about supplements and diets for gut health that aren’t backed by strong evidence.
What is the microbiome?
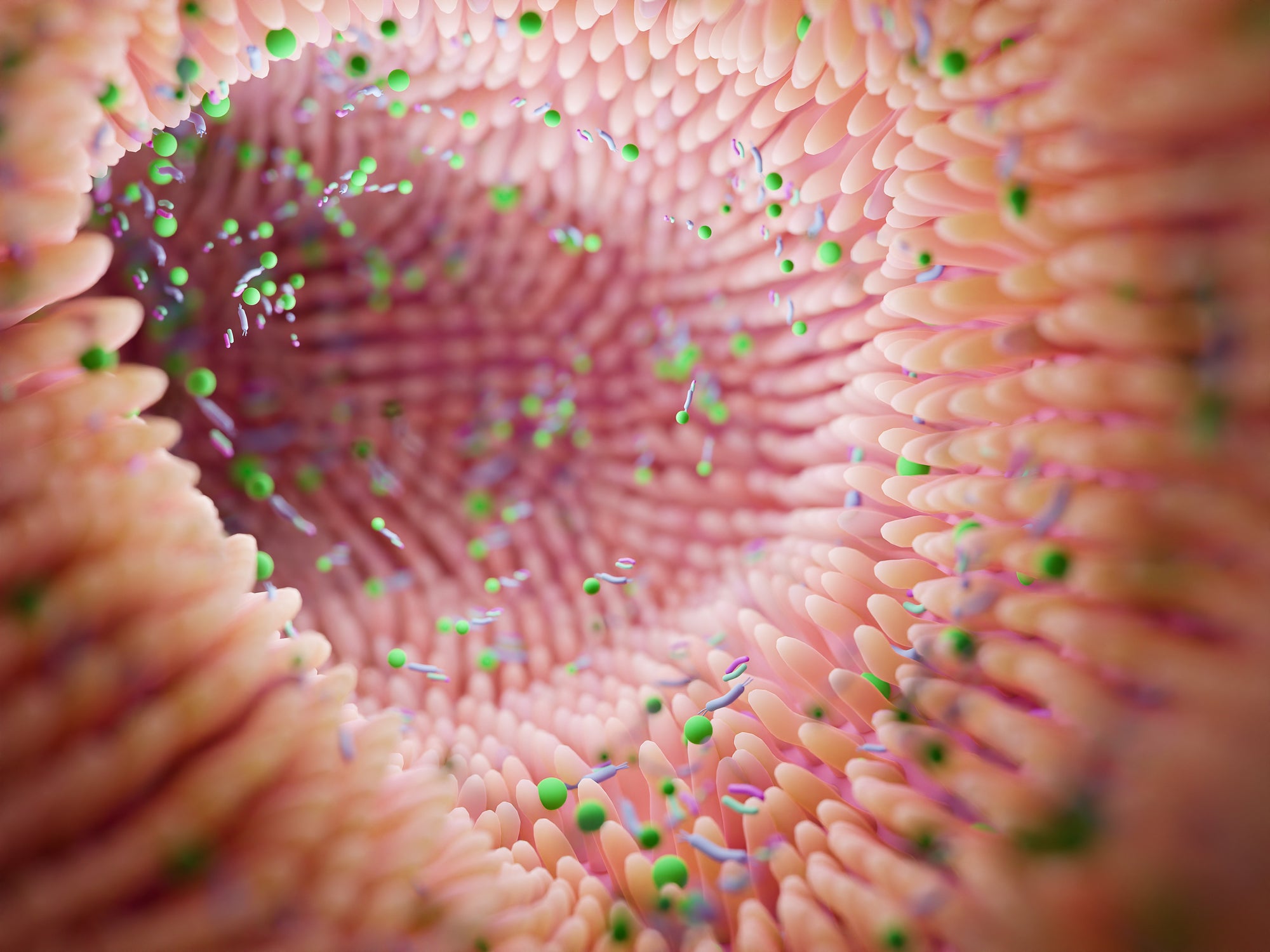
The microbiome is the community of microbes found in the body. Technically, microbiome refers to collective genomes of these microbes with microbiota used to describe the communities of microbes but in general use, these terms are used synonymously. Usually, the microbiome in common usage refers to the community of bacteria in the gut but it also includes other microbes like fungi, protozoa, and viruses and there is distinct microbiota of the skin, oral cavity, and other surfaces.

What are probiotics?
Probiotics are microbes (usually bacteria) that can be taken as a supplement to help improve the balance of the microbiome.
What are prebiotics?
Prebiotics are fuels that feed (beneficial) microbes in the gut. Usually, these are fibers and resistant starches that feed particular bacteria.
Effects of the gut on health
Gut health and the microbiome play an important role in our overall health. Poor gut health caused by disturbances to the balance of good and bad microbes in the gut can affect both nourishment and growth and metabolic conditions like obesity and type 2 diabetes.1
Nourishment and gut health
The key role of the gastrointestinal tract is to absorb nutrients from food. So, having a gut that functions correctly and absorb nutrients from food is essential to achieving optimal health. The microbiome also contains bacteria that produce nutrients, like short-chain fatty acids that feed cells of the digestive wall, other bacteria, and can be taken up into the body to use as fuel. These and other chemicals produced by bacteria in the gut also act as messengers that provide a metabolic interaction between the host (you) and the microbiota and digestive environment.2

Inflammation and immunity and gut health
Far more than just being an organ to absorb nutrition, the gut is essential for the regulation of systemic inflammation, and plays a role in inflammatory conditions like psoriasis.3 Interestingly, in people with inflammatory conditions, there is typically a reduced diversity and abundance of bacteria in the gut,4-6 and reduced diversity and abundance of bacteria in the gut is also associated with increased inflammation.7
The gut-brain link and the effects of gut-health on mental health (and vice versa!)
The gut and brain are linked, and this has led some to call the gut the second brain. Mental health challenges were once considered to be structural problems or functional neurotransmitter imbalances within the brain, it is now known that overall health, inflammation, and gut-health play a role in the health of the brain, nervous system, and the psyche of an individual.8
Depression and gut health
Recent research indicates that depression is both an inflammatory disease and that there is communication between the gut and the brain and nervous system and that this is related to depression. Animal research has shown that when the faecal microbiome from animals showing depressive signs is transplanted into non-depressed subjects, they develop depressive symptoms, and most reported studies have shown a correlation between the gut microbiota and depression,9 although a 2020 meta-analysis showed no clear effect of either prebiotic or probiotic supplements.10
Anxiety and gut health
Recent research suggests that the microbiome plays a role in regulating mood, anxiety, and stress.11 Anxiety and depression, and irritable bowel syndrome (IBS) are also common, and around 40-90% of those with anxiety share these conditions. Human and animal trials indicate that people with IBS and anxiety have a reduced diversity of bacteria and higher abundance of Proteobacteria, Prevotella/Prevotellaceae, Bacteroides and lower levels of Lachnospiraceae relative to healthy controls.12
Key points:
- Gut and brain and nervous system health are linked.
- Gut health is likely to play an important role in depression and anxiety.
Gut health and sleep
Poor sleep might also affect gut-health, contributing to an inflammatory state and metabolic diseases.13,14 Chemical messengers from the gut microbiome also help to influence circadian rhythms (day-night/sleep-wake cycles) and help to regulate sleep, metabolism, and body composition and both disturbed and short sleep are associated with gut dysbiosis. Additionally, the end products of bacterial species which grow in response to sleep loss can induce fatigue. Furthermore, probiotic supplementation has been found to improve sleep quality.15
Disturbed sleep is known to worsen eating behaviors and may play a role in the disturbance to the microbiota seen with poor sleep. Animal and human research have shown that disturbed sleep increases food intake and changes the microbiota, leading to inflammation and insulin resistance.16 Antibiotics (which reduce bacteria number and diversity) have also been shown to reduce sleep in mice,17 while research in people with IBS also suggests that gut dysfunction affects sleep.18 However, in a study of young, active adults (18-35 years) no significant relationship between habitual sleep duration and microbiota diversity was observed.19

Key points:
- Poor gut health affects sleep and poor sleep affects gut health.
- Probiotics might help to improve sleep quality.
Gut health and skin health
The connection between gut and skin health has been known for some time. Many conditions of the skin such as psoriasis and eczema result from a combination of factors, which include allergy and inflammation and so, the barrier and immune functions of the gut are important for skin health.
Gut health and acne
Acne is an inflammatory skin condition and for nearly a century the link between the gut, brain, and skin has been suggested.20 The gut microbiome is also important for this condition, as it affects immunity, inflammation and intestinal permeability, contributing to skin inflammation.21 Research shows that people with acne have different microbiota to those without acne.22 While changes in diet have typically been considered to have little effect on acne, clinical experience suggests otherwise. It is now suggested that diets that reduce inflammation and support a healthy microbiome, including those based on natural, unrefined foods and with plenty of gut-supporting fiber and resistant starch, be considered for acne.23
Gut health and eczema
Eczema is a common inflammatory condition of the skin affecting around 1 in 10 people at some point in their lives. Increasingly, studies are demonstrating a link between the gut microbiome and eczema.24 A significant proportion of children who develop food sensitivities go on to develop food allergies and eczema, and these anomalous immune responses are thought to be linked to the gut-immune axis of the body.25 Children with eczema also have lower bacterial diversity than those without,26-30 and different microbiome signatures.31-41
There is some debate about the role that probiotics might play in eczema. Overall, systematic reviews of the literature suggest a 26% reduction in risk for eczema with probiotic supplementation.42 Prebiotics can also be beneficial for correcting the microbiome, especially for formula-fed infants.43-45
Gut health and psoriasis
The gut-skin axis is thought to be related to the immune-inflammatory cascade and there is an increased prevalence of psoriasis and psoriatic arthritis with inflammatory bowel disease.46 The gut microbiota of patients with psoriasis show reduced diversity,47 and a distinct signature compared to controls.48
Key points:
- People with inflammatory skin conditions have different microbiota to those without these skin conditions.
- The gut microbiome is important for regulating inflammation throughout the body.
- Probiotics might help inflammatory skin conditions such as eczema.
Can gut health cause hair loss?
Hair loss can be due to genetic disposition (male pattern baldness), micronutrient deficiencies (such as a zinc deficiency) or to an autoimmune inflammatory disorder such as alopecia areata. In the case of alopecia, the gut biome is thought to play a similar role as it does in other inflammatory disorders,49 and people with alopecia are also likely to have different microbiome signatures than healthy controls.50
Can gut health affect blood pressure?
Blood pressure may also be partially mediated by the gut microbiome,51-54 along with gut health being associated with metabolic health which also causes high blood pressure. High intakes of fruit, vegetables, and fiber that are known to support the microbiome (by feeding beneficial bacteria) also result in short-chain fatty acids being produced by those bacteria. These short-chain fatty acids are linked to lower blood pressure.55-58 Chronic inflammation and “leaky gut” are also associated with blood pressure.59
Can gut health cause headaches?
The gut-brain axis is thought to play a role in the causation of migraines and headache.60 However, the reasons for this aren’t entirely clear. It is thought that a range of factors, from inflammation to pain signaling, blood pressure regulation, and other gut-related cell-signals could all be at play in the gut-headache relationship.61-63
While several randomized trials have shown reduced frequency and severity of migraine attacks with probiotic supplement use64, 65 (without changes in inflammation or intestinal permeability), a systematic review of the available trials published in 2020 found no significant effect of probiotic supplementation on migraines.66

How does gut health affect hormones?
The gut and microbiome play a role in the metabolism and clearance of various hormones such as oestrogen,67, 68 and oestrogen itself has an interrelationship with the gut-brain axis.69 This is important because oestrogen sensitive cancers are a significant risk, especially in postmenopausal women,70 and alterations to the gut microbiome that affect oestrogen regulation in the body could drive oestrogen-related illnesses.71Animal research also suggests a role for oestrogen inhibiting menopausal symptoms and preserving microbiome diversity.72,73
Testosterone function in males could also be affected by poor gut health. Overweight and obesity are associated with poorer gut health and endotoxin damage. In a study looking at the effects of these on testosterone, body fat was correlated with both endotoxins and inflammation and reduced testosterone.74 Animal research had previously demonstrated reduced testosterone production (and increased risk of obesity) resulting from the antibiotics doxycycline and ciprofloxacin,75, 76 that was improved by probiotics.75
Key points:
- The microbiome helps process and eliminate steroid hormones.
- Disturbances to the microbiome could worsen oestrogen-related illnesses and cancers in women.
- The microbiome might affect optimal testosterone levels in men.
Does gut health affect weight loss?
The gut microbiome plays a role in hunger, satiety, and inflammation and there is a complex relationship with weight management. Emerging research suggests that there are distinct microbiome signatures associated with obesity,77 and with cardiometabolic states also associated with overweight and obesity, in particular, systemic inflammation.7
Gut health, diabetes, and cardiometabolic health
The gut biome has a bidirectional relationship with hunger, satiety, inflammation and immunity, all of which interplay with the spectrum of acquired ‘diabesity’,78 and there is also likely to be involvement of the gut and microbiota with Type 1 (autoimmune) diabetes.79, 80
Reviews of the evidence suggest that supplementation with probiotics in diabetes and metabolic disorder benefits blood glucose control, lipids, insulin levels and sensitivity, and inflammation.81-89
Cardiovascular health
The microbiome and gut health Intestinal microbiota are linked to cardiovascular health and modifying the gut environment might help to prevent cardiovascular disease.7, 90
Use of probiotics is also linked to reductions in blood pressure,91 a marker of heart disease and reductions in inflammatory endotoxins92, 93 (toxins created within the body, usually by the breakdown of “bad” bacteria in the gut and the uptake of these into the body because of poor gut health), which also contribute to cardiometabolic diseases like heart disease, obesity, and diabetes.
Key points:
- The microbiome affects inflammation, food intake, and various measures of cardiometabolic health.
- The microbiome is likely affected by a poor diet and other lifestyle factors that contribute to metabolic disease and obesity.
- The microbiome and gut health also cause conditions in the body related to metabolic health and obesity.
- Probiotics may be beneficial for metabolic disease.
Are protein powders good for gut health?
Generally, the focus on nutrients for gut health falls on fibers, resistant starches, and fatty acids from fish oil, dairy, palm or coconut oils. Fermentation of excessive protein in the gut might contribute to dysbiosis and worsen gut health, but animal research suggests these effects are mitigated by increased fiber intake,94 (in other words, this isn’t likely to be an issue in a balanced diet) and few people over-consume protein in any event. In fact, the bigger issue for most people is not whether they consume too much protein, but that they don’t take in enough to thrive. Protein is critical to health, performance, and adherence to a good diet and so, taking supplementing your diet with a powder (like Clean Lean Protein) can help to support health, and by extension, gut health.

Are probiotics good for gut health?
The research on probiotics is conflicting and there will be differences in results based on which species and strains of bacteria are used for which outcomes. Overall though, the accumulated evidence suggests that probiotic supplements can be useful for:
- Dysbiosis95, 96
- Dysbiosis in HIV97
- Reducing inflammation and allergy98
- Diarrhea, constipation, pain and bloating, symptoms of lactose intolerance, 99-102
- Inflammatory bowel disease103
- Improved sleep15
- Eczema42
- Migraine64, 65
- Possible improvement in both male and female hormone balance73, 75
- Diabetes and metabolic syndrome81-89
- Cardiovascular health91-93
There are different microbiome signatures associated with poor health and with different health conditions and so, specific strains may be more or less useful for particular conditions. If you require specific treatment for a health condition or disorder, see a qualified practitioner who is well-versed in gut-health.
Other nutrients for a healthy gut
It is now known that the health of the gut has a big effect on the health of other organs and systems and particular focus has fallen on the interplay of gut-health with that of the brain and nervous system, and the skin. As with any other body system, the foundation of nutrition for gut health is a diet that is packed with essential nutrients, and that provides sufficient energy, protein, and essential fats. Specifically, the gut also benefits from sufficient amounts of prebiotic starches and fibers from foods like legumes, grains, and vegetables, that feed “good” bacteria in the gut,104 along with omega-3 fats,105 and short- and medium-chain fats that aid the balance of the microbiome (the community of microbes) in the gut.106, 107
Also, many nutrients have been shown to help support gut health, such as:
- Plant phenols and antioxidants – Health-promoting compounds in plants that work together with probiotics to improve the balance of the microbiome. 108 Preclinical trials also provide evidence for the traditional use of the fruit Rosehip improved gastrointestinal health. 109, 110
- Digestive and tonic herbs – Bitter greens (like dandelion) with anti-inflammatory and antioxidant actions. 111, 112
- Ginger – Known to reduce nausea (especially during pregnancy) 113-116
- Adaptogenic herbs, especially Astragalus which offers protection against intestinal inflammation. 117
- Soothing herbs such as slippery elm, considered to be soothing and anti-inflammatory and used as a digestive aid. 118, 119
- Anti-inflammatory spices like turmeric 120, 121
- Zinc – an important mineral for the gut because it helps to close ‘tight junctions’ in the gut wall, reducing the potential for allergens and pathogens to enter the body. 122, 123 Note: many people do not get enough zinc from diet alone.
Lifestyle and gut health
Exercise and gut health
Exercise is associated with greater diversity and health of the microbiome of the gut,124, 125 and benefits are likely to be greater with improved body composition.126, 127

Stress and gut health
Stress is a common, yet often overlooked factor in the health of the gut. Severe trauma (PTSD) is associated with an increased likelihood of developing IBS,128 as is stress overall, and other types of stressful life events.129 Additionally, mindfulness meditation reduces the severity of IBS.130
Other factors that can affect the health of the gut:
- Poor sleep
- Smoking
- Excessive alcohol use
Interestingly, the combination of probiotics with plant phenols provides synergistic benefits, with greater survival, adhesion, and maintenance of beneficial bacteria and improved health benefits. 108
Do sweeteners harm the microbiome?
While some experimental animal studies have suggested the non-nutritive sweeteners can worsen blood glucose control, increase food consumption, and cause weight gain (possibly due to effects on the microbiome), the evidence from human studies suggests that have little if any effect. Meta-analyses (studies compiling data from many trials) have shown that non-nutritive sweeteners have little or no effect on blood glucose control in humans,131 or on gut health,132 and few negative functional effects on the human gut have been observed.132 Erythritol, in particular, does not appear to be fermentable by colonic bacteria and is unlikely to have any effect on the gut microbiome.133
Relationship between gut health and overall health
The gut is intricately linked to the health of the entire body and every one of its systems. The relationship between gut health and the health of the body is bi-directional, meaning that one affects the other and vice versa. At this time much of the research is preliminary and especially with probiotic treatments, there are distinct differences between conditions, individuals, and their microbiota and therefore, the probiotic treatments that may be beneficial. But, on balance, broad-spectrum lactobacillus and bifidobacteria are beneficial to health, as are increased fiber intakes, along with other nutrients derived from a diet rich in vegetables, berries, and spices and herbs, and fermented foods. Exercise, mindfulness, sleep, and stress reduction also each play an interrelated role in the health of the gut and body.
References
- Wilson AS, Koller KR, Ramaboli MC, Nesengani LT, Ocvirk S, Chen C, et al. Diet and the Human Gut Microbiome: An International Review. Digest Dis Sci. 2020;65(3):723-40.
- Yadav M, Verma MK, Chauhan NS. A review of metabolic potential of human gut microbiome in human nutrition. Archives of Microbiology. 2018;200(2):203-17.
- Damiani G, Bragazzi NL, McCormick TS, Pigatto PDM, Leone S, Pacifico A, et al. Gut microbiota and nutrient interactions with skin in psoriasis: A comprehensive review of animal and human studies. World J Clin Cases. 2020;8(6):1002.
- Hidalgo-Cantabrana C, Gómez J, Delgado S, Requena-López S, Queiro-Silva R, Margolles A, et al. Gut microbiota dysbiosis in a cohort of patients with psoriasis. British Journal of Dermatology. 2019;181(6):1287-95.
- Alesa DI, Alshamrani HM, Alzahrani YA, Alamssi DN, Alzahrani NS, Almohammadi ME. The role of gut microbiome in the pathogenesis of psoriasis and the therapeutic effects of probiotics. J Family Med Prim Care. 2019;8(11):3496-503.
- Coit P, Sawalha AH. The human microbiome in rheumatic autoimmune diseases: A comprehensive review. Clinical Immunology. 2016;170:70-9.
- van den Munckhof ICL, Kurilshikov A, ter Horst R, Riksen NP, Joosten LAB, Zhernakova A, et al. Role of gut microbiota in chronic low-grade inflammation as potential driver for atherosclerotic cardiovascular disease: a systematic review of human studies. Obesity Reviews. 2018;19(12):1719-34.
- Hélѐne-Zanin J. Gut feelings: a thematic review of the links between acute gastrointestinal illness and anxiety and depressive disorders. Global Health: Annual Review. 2015;1(1).
- Yang Z, Li J, Gui X, Shi X, Bao Z, Han H, et al. Updated review of research on the gut microbiota and their relation to depression in animals and human beings. Molecular Psychiatry. 2020.
- Vaghef-Mehrabany E, Maleki V, Behrooz M, Ranjbar F, Ebrahimi-Mameghani M. Can psychobiotics “mood” ify gut? An update systematic review of randomized controlled trials in healthy and clinical subjects, on anti-depressant effects of probiotics, prebiotics, and synbiotics. Clinical Nutrition. 2020;39(5):1395-410.
- Yang B, Wei J, Ju P, Chen J. Effects of regulating intestinal microbiota on anxiety symptoms: A systematic review. Gen Psychiatr. 2019;32(2):e100056-e.
- Simpson CA, Mu A, Haslam N, Schwartz OS, Simmons JG. Feeling down? A systematic review of the gut microbiota in anxiety/depression and irritable bowel syndrome. Journal of Affective Disorders. 2020;266:429-46.
- Reynolds AC, Paterson JL, Ferguson SA, Stanley D, Wright Jr KP, Dawson D. The shift work and health research agenda: considering changes in gut microbiota as a pathway linking shift work, sleep loss and circadian misalignment, and metabolic disease. Sleep medicine reviews. 2017;34:3-9.
- Parekh PJ, Oldfield ECIV, Johnson DA. The Effects of Sleep on the Commensal Microbiota: Eyes Wide Open? Journal of Clinical Gastroenterology. 2018;52(3).
- Matenchuk BA, Mandhane PJ, Kozyrskyj AL. Sleep, Circadian Rhythm, and Gut Microbiota. Sleep Medicine Reviews. 2020:101340.
- Poroyko VA, Carreras A, Khalyfa A, Khalyfa AA, Leone V, Peris E, et al. Chronic Sleep Disruption Alters Gut Microbiota, Induces Systemic and Adipose Tissue Inflammation and Insulin Resistance in Mice. Scientific Reports. 2016;6(1):35405.
- Lendrum JE, Seebach B, Klein B, Liu S. Sleep and the gut microbiome: antibiotic-induced depletion of the gut microbiota reduces nocturnal sleep in mice. BioRxiv. 2017:199075.
- Orr WC, Crowell MD, Lin B, Harnish MJ, Chen JDZ. Sleep and gastric function in irritable bowel syndrome: derailing the brain-gut axis. Gut. 1997;41(3):390.
- Morales Marroquín FE. Distal gut microbiome association with sleep duration and quality 2018.
- Bowe WP, Logan AC. Acne vulgaris, probiotics and the gut-brain-skin axis - back to the future? Gut Pathogens. 2011;3(1):1.
- Lee YB, Byun EJ, Kim HS. Potential Role of the Microbiome in Acne: A Comprehensive Review. Journal of Clinical Medicine. 2019;8(7):987.
- Yan H-M, Zhao H-J, Guo D-Y, Zhu P-Q, Zhang C-L, Jiang W. Gut microbiota alterations in moderate to severe acne vulgaris patients. The Journal of Dermatology. 2018;45(10):1166-71.
- Clark AK, Haas KN, Sivamani RK. Edible Plants and Their Influence on the Gut Microbiome and Acne. International Journal of Molecular Sciences. 2017;18(5):1070.
- Köberle M, Biedermann T. [Microbiome, atopic eczema and blockade of type 2 immunity]. Der Hautarzt; Zeitschrift fur Dermatologie, Venerologie, und verwandte Gebiete. 2018;69(3):197-203.
- Marrs T, Flohr C. How do Microbiota Influence the Development and Natural History of Eczema and Food Allergy? The Pediatric Infectious Disease Journal. 2016;35(11):1258-61.
- Wang M, Karlsson C, Olsson C, Adlerberth I, Wold AE, Strachan DP, et al. Reduced diversity in the early fecal microbiota of infants with atopic eczema. Journal of Allergy and Clinical Immunology. 2008;121(1):129-34.
- Forno E, Onderdonk AB, McCracken J, Litonjua AA, Laskey D, Delaney ML, et al. Diversity of the gut microbiota and eczema in early life. Clinical and Molecular Allergy. 2008;6(1):11.
- Abrahamsson TR, Jakobsson HE, Andersson AF, Björkstén B, Engstrand L, Jenmalm MC. Low diversity of the gut microbiota in infants with atopic eczema. Journal of Allergy and Clinical Immunology. 2012;129(2):434-40.e2.
- Diversity of the Gut Microbiota and Eczema in Infants. D47 NEONATAL AND RARE LUNG DISEASES. p. A5981.
- Ismail IH, Oppedisano F, Joseph SJ, Boyle RJ, Licciardi PV, Robins-Browne RM, et al. Reduced gut microbial diversity in early life is associated with later development of eczema but not atopy in high-risk infants. Pediatric Allergy and Immunology. 2012;23(7):674-81.
- Nylund L, Satokari R, Nikkilä J, Rajilić-Stojanović M, Kalliomäki M, Isolauri E, et al. Microarray analysis reveals marked intestinal microbiota aberrancy in infants having eczema compared to healthy children in at-risk for atopic disease. BMC Microbiology. 2013;13(1):12.
- Tang MF, Sy HY, Kwok JSL, Tam WH, Hon KL, Tung CKC, et al. Eczema susceptibility and composition of faecal microbiota at 4 weeks of age: a pilot study in Chinese infants. British Journal of Dermatology. 2016;174(4):898-900.
- Zimmermann P, Messina N, Mohn WW, Finlay BB, Curtis N. Association between the intestinal microbiota and allergic sensitization, eczema, and asthma: A systematic review. Journal of Allergy and Clinical Immunology. 2019;143(2):467-85.
- Zhang Y, Jin S, Wang J, Zhang L, Mu Y, Huang K, et al. Variations in early gut microbiome are associated with childhood eczema. FEMS Microbiology Letters. 2019;366(9).
- Wang H, Li Y, Feng X, Li Y, Wang W, Qiu C, et al. Dysfunctional gut microbiota and relative co-abundance network in infantile eczema. Gut Pathogens. 2016;8(1):36.
- Penders J, Stobberingh EE, Thijs C, Adams H, Vink C, Van Ree R, et al. Molecular fingerprinting of the intestinal microbiota of infants in whom atopic eczema was or was not developing. Clinical & Experimental Allergy. 2006;36(12):1602-8.
- Zheng H, Liang H, Wang Y, Miao M, Shi T, Yang F, et al. Altered Gut Microbiota Composition Associated with Eczema in Infants. PloS one. 2016;11(11):e0166026-e.
- Mah KW, Björkstén B, Lee BW, van Bever HP, Shek LP, Tan TN, et al. Distinct Pattern of Commensal Gut Microbiota in Toddlers with Eczema. International Archives of Allergy and Immunology. 2006;140(2):157-63.
- West CE, Rydén P, Lundin D, Engstrand L, Tulic MK, Prescott SL. Gut microbiome and innate immune response patterns in IgE-associated eczema. Clinical & Experimental Allergy. 2015;45(9):1419-29.
- Ismail IH, Boyle RJ, Licciardi PV, Oppedisano F, Lahtinen S, Robins-Browne RM, et al. Early gut colonization by Bifidobacterium breve and B. catenulatum differentially modulates eczema risk in children at high risk of developing allergic disease. Pediatric Allergy and Immunology. 2016;27(8):838-46.
- Gore C, Munro K, Lay C, Bibiloni R, Morris J, Woodcock A, et al. Bifidobacterium pseudocatenulatum is associated with atopic eczema: A nested case-control study investigating the fecal microbiota of infants. Journal of Allergy and Clinical Immunology. 2008;121(1):135-40.
- Mansfield JA, Bergin SW, Cooper JR, Olsen CH. Comparative Probiotic Strain Efficacy in the Prevention of Eczema in Infants and Children: A Systematic Review and Meta-Analysis. Military Medicine. 2014;179(6):580-92.
- Wopereis H, Sim K, Shaw A, Warner JO, Knol J, Kroll JS. Intestinal microbiota in infants at high risk for allergy: Effects of prebiotics and role in eczema development. Journal of Allergy and Clinical Immunology. 2018;141(4):1334-42.e5.
- Holscher HD, Faust KL, Czerkies LA, Litov R, Ziegler EE, Lessin H, et al. Effects of prebiotic-containing infant formula on gastrointestinal tolerance and fecal microbiota in a randomized controlled trial. JPEN Journal of Parenteral & Enteral Nutrition. 2012;36(1 Suppl):95S-105s.
- Holscher HD, Bauer LL, Gourineni V, Pelkman CL, Fahey Jr GC, Swanson KS. Agave Inulin Supplementation Affects the Fecal Microbiota of Healthy Adults Participating in a Randomized, Double-Blind, Placebo-Controlled, Crossover Trial. Journal of Nutrition. 2015;145(9):2025-32.
- Myers B, Brownstone N, Reddy V, Chan S, Thibodeaux Q, Truong A, et al. The gut microbiome in psoriasis and psoriatic arthritis. Best Practice & Research Clinical Rheumatology. 2020:101494.
- Hidalgo‐Cantabrana C, Gomez J, Delgado S, Requena‐López S, Queiro‐Silva R, Margolles A, et al. Gut microbiota dysbiosis in a cohort of patients with psoriasis. British Journal of Dermatology. 2019;181(6):1287-95.
- Codoñer FM, Ramírez-Bosca A, Climent E, Carrión-Gutierrez M, Guerrero M, Pérez-Orquín JM, et al. Gut microbial composition in patients with psoriasis. Scientific Reports. 2018;8(1):3812.
- Borde A, Åstrand A. Alopecia areata and the gut—the link opens up for novel therapeutic interventions. Expert Opinion on Therapeutic Targets. 2018;22(6):503-11.
- Moreno-Arrones OM, Serrano-Villar S, Perez-Brocal V, Saceda-Corralo D, Morales-Raya C, Rodrigues-Barata R, et al. Analysis of the gut microbiota in alopecia areata: identification of bacterial biomarkers. Journal of the European Academy of Dermatology and Venereology. 2020;34(2):400-5.
- Jama HA, Kaye DM, Marques FZ. The gut microbiota and blood pressure in experimental models. Current Opinion in Nephrology and Hypertension. 2019;28(2).
- Raizada MK, Joe B, Bryan NS, Chang EB, Dewhirst FE, Borisy GG, et al. Report of the National Heart, Lung, and Blood Institute Working Group on the Role of Microbiota in Blood Pressure Regulation. Hypertension. 2017;70(3):479-85.
- Al Khodor S, Reichert B, Shatat IF. The Microbiome and Blood Pressure: Can Microbes Regulate Our Blood Pressure? Frontiers in Pediatrics. 2017;5(138).
- Yang T, Zubcevic J. Gut–Brain Axis in Regulation of Blood Pressure. Frontiers in Physiology. 2017;8(845).
- Marques FZ, Mackay CR, Kaye DM. Beyond gut feelings: how the gut microbiota regulates blood pressure. Nature Reviews Cardiology. 2018;15(1):20-32.
- Ufnal M, Onyszkiewicz M, Gawrys M, Huc T, Aleksandrowicz M, Sawicka A, et al. Butyric Acid, a Gut Bacteria-Produced Metabolite, Decreases Arterial Blood Pressure via a Gut-Vagus Nerve Signaling in Rats. The FASEB Journal. 2019;33(1_supplement):516.8-.8.
- Natarajan N, Hori D, Flavahan S, Steppan J, Flavahan NA, Berkowitz DE, et al. Gut Microbiota in Health and Disease: Microbial short chain fatty acid metabolites lower blood pressure via endothelial G protein-coupled receptor 41. Physiological Genomics. 2016;48(11):826.
- Poll B, Steppan J, Lester L, Berkowitz D, Pluznick J. A short chain fatty acid produced by the gut microbiota plays a role in blood pressure regulation and cardiac contractility. The FASEB Journal. 2019;33(1_supplement):569.19-.19.
- Kim S, Goel R, Kumar A, Qi Y, Lobaton G, Hosaka K, et al. Imbalance of gut microbiome and intestinal epithelial barrier dysfunction in patients with high blood pressure. Clinical Science. 2018;132(6):701-18.
- Hindiyeh N, Aurora SK. What the Gut Can Teach Us About Migraine. Current Pain and Headache Reports. 2015;19(7):33.
- Arzani M, Jahromi SR, Ghorbani Z, Vahabizad F, Martelletti P, Ghaemi A, et al. Gut-brain Axis and migraine headache: a comprehensive review. The Journal of Headache and Pain. 2020;21(1):1-12.
- Tang Y, Liu S, Shu H, Yanagisawa L, Tao F. Gut Microbiota Dysbiosis Enhances Migraine-Like Pain Via TNFα Upregulation. Molecular Neurobiology. 2020;57(1):461-8.
- Chen J, Wang Q, Wang A, Lin Z. Structural and Functional Characterization of the Gut Microbiota in Elderly Women With Migraine. Frontiers in Cellular and Infection Microbiology. 2020;9(470).
- Martami F, Togha M, Seifishahpar M, Ghorbani Z, Ansari H, Karimi T, et al. The effects of a multispecies probiotic supplement on inflammatory markers and episodic and chronic migraine characteristics: A randomized double-blind controlled trial. Cephalalgia. 2019;39(7):841-53.
- De Roos N, Van Hemert S, Rovers J, Smits M, Witteman B. The effects of a multispecies probiotic on migraine and markers of intestinal permeability–results of a randomized placebo-controlled study. European journal of clinical nutrition. 2017;71(12):1455-62.
- Parohan M, Djalali M, Sarraf P, Yaghoubi S, Seraj A, Foroushani AR, et al. Effect of probiotic supplementation on migraine prophylaxis: a systematic review and meta-analysis of randomized controlled trials. Nutritional neuroscience. 2020:1-8.
- Parida S, Sharma D. The Microbiome–Estrogen Connection and Breast Cancer Risk. Cells. 2019;8(12):1642.
- Fuhrman BJ, Feigelson HS, Flores R, Gail MH, Xu X, Ravel J, et al. Associations of the Fecal Microbiome With Urinary Estrogens and Estrogen Metabolites in Postmenopausal Women. The Journal of Clinical Endocrinology & Metabolism. 2014;99(12):4632-40.
- Jiang Y, Meerveld BG-V, Johnson AC, Travagli RA. Role of estrogen and stress on the brain-gut axis. American Journal of Physiology-Gastrointestinal and Liver Physiology. 2019;317(2):G203-G9.
- Kwa M, Plottel CS, Blaser MJ, Adams S. The Intestinal Microbiome and Estrogen Receptor–Positive Female Breast Cancer. JNCI: Journal of the National Cancer Institute. 2016;108(8).
- Baker JM, Al-Nakkash L, Herbst-Kralovetz MM. Estrogen–gut microbiome axis: physiological and clinical implications. Maturitas. 2017;103:45-53.
- Park S, Kim DS, Kang ES, Kim DB, Kang S. Low-dose brain estrogen prevents menopausal syndrome while maintaining the diversity of the gut microbiomes in estrogen-deficient rats. American Journal of Physiology-Endocrinology and Metabolism. 2018;315(1):E99-E109.
- Jeong S-Y, Kang S, Hua CS, Ting Z, Park S. Synbiotic effects of β-glucans from cauliflower mushroom and Lactobacillus fermentum on metabolic changes and gut microbiome in estrogen-deficient rats. Genes & nutrition. 2017;12(1):31.
- Tremellen K, McPhee N, Pearce K, Benson S, Schedlowski M, Engler H. Endotoxin-initiated inflammation reduces testosterone production in men of reproductive age. American journal of physiology Endocrinology and metabolism. 2018;314(3):E206-E13.
- Xie C, Bian Y, Feng H, Zhao Y, Wang L, Li Y, et al. Reversal of ciprofloxacin-induced testosterone reduction by probiotic microbes in mouse testes. General and Comparative Endocrinology. 2019;284:113268.
- Hou X, Zhu L, Zhang X, Zhang L, Bao H, Tang M, et al. Testosterone disruptor effect and gut microbiome perturbation in mice: Early life exposure to doxycycline. Chemosphere. 2019;222:722-31.
- Villanueva-Millán M, Perez-Matute P, Oteo J. Gut microbiota: a key player in health and disease. A review focused on obesity. Journal of physiology and biochemistry. 2015;71(3):509-25.
- Singer-Englar T, Barlow G, Mathur R. Obesity, diabetes, and the gut microbiome: an updated review. Expert review of gastroenterology & hepatology. 2019;13(1):3-15.
- Zheng P, Li Z, Zhou Z. Gut microbiome in type 1 diabetes: A comprehensive review. Diabetes/metabolism research and reviews. 2018;34(7):e3043.
- Jamshidi P, Hasanzadeh S, Tahvildari A, Farsi Y, Arbabi M, Mota JF, et al. Is there any association between gut microbiota and type 1 diabetes? A systematic review. Gut pathogens. 2019;11(1):49.
- Tabrizi R, Ostadmohammadi V, Lankarani KB, Akbari M, Akbari H, Vakili S, et al. The effects of probiotic and synbiotic supplementation on inflammatory markers among patients with diabetes: A systematic review and meta-analysis of randomized controlled trials. European journal of pharmacology. 2019.
- Kesika P, Sivamaruthi BS, Chaiyasut C. Do Probiotics Improve the Health Status of Individuals with Diabetes Mellitus? A Review on Outcomes of Clinical Trials. BioMed Research International. 2019;2019:1531567.
- Hajifaraji M, Dolatkhah N. Probiotics and Metabolic Outcomes of Gestational Diabetes: A Review Article. Journal of Mazandaran University of Medical Sciences. 2018;28(162):155-74.
- Homayouni A, Bagheri N, Mohammad-Alizadeh-Charandabi S, Kashani N, Mobaraki-Asl N, Mirghafurvand M, et al. Prevention of Gestational Diabetes Mellitus (GDM) and Probiotics: Mechanism of action: A Review. Curr Diabetes Rev. 2019.
- Pan J, Pan Q, Chen Y, Zhang H, Zheng X. Efficacy of probiotic supplement for gestational diabetes mellitus: a systematic review and meta-analysis. The Journal of Maternal-Fetal & Neonatal Medicine. 2019;32(2):317-23.
- Dallanora S, de Souza YM, Deon RG, Tracey CA, Freitas-Vilela AA, Roesch LFW, et al. Do probiotics effectively ameliorate glycemic control during gestational diabetes? A systematic review. Archives of gynecology and obstetrics. 2018;298(3):477-85.
- Tiderencel KA, Hutcheon DA, Ziegler J. Probiotics for the treatment of type 2 diabetes: A review of randomized controlled trials. Diabetes/Metabolism Research and Reviews. 2020;36(1):e3213.
- Sáez-Lara MJ, Robles-Sanchez C, Ruiz-Ojeda FJ, Plaza-Diaz J, Gil A. Effects of Probiotics and Synbiotics on Obesity, Insulin Resistance Syndrome, Type 2 Diabetes and Non-Alcoholic Fatty Liver Disease: A Review of Human Clinical Trials. International Journal of Molecular Sciences. 2016;17(6):928.
- Koutnikova H, Genser B, Monteiro-Sepulveda M, Faurie J-M, Rizkalla S, Schrezenmeir J, et al. Impact of bacterial probiotics on obesity, diabetes and non-alcoholic fatty liver disease related variables: a systematic review and meta-analysis of randomised controlled trials. BMJ open. 2019;9(3):e017995.
- Tang WHW, Bäckhed F, Landmesser U, Hazen SL. Intestinal Microbiota in Cardiovascular Health and Disease: JACC State-of-the-Art Review. Journal of the American College of Cardiology. 2019;73(16):2089-105.
- Hendijani F, Akbari V. Probiotic supplementation for management of cardiovascular risk factors in adults with type II diabetes: A systematic review and meta-analysis. Clinical Nutrition. 2018;37(2):532-41.
- March DS, Jones AW, Bishop NC, Burton JO. The Efficacy of Prebiotic, Probiotic, and Synbiotic Supplementation in Modulating Gut-Derived Circulatory Particles Associated With Cardiovascular Disease in Individuals Receiving Dialysis: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Journal of Renal Nutrition. 2019.
- Moludi J, Maleki V, Jafari-Vayghyan H, Vaghef-Mehrabany E, Alizadeh M. Metabolic endotoxemia and cardiovascular disease: A systematic review about potential roles of prebiotics and probiotics. Clinical and Experimental Pharmacology and Physiology. 2020;47(6):927-39.
- Jha R, Berrocoso JF. Dietary fiber and protein fermentation in the intestine of swine and their interactive effects on gut health and on the environment: A review. Animal Feed Science and Technology. 2016;212:18-26.
- Mahmood Fashandi H, Abbasi R, Mousavi Khaneghah A. The detoxification of aflatoxin M1 by Lactobacillus acidophilus and Bifidobacterium spp.: A review. Journal of Food Processing and Preservation. 2018;42(9):e13704.
- Dinev T, Beev G, Denev S, Dermendzhieva D, Tzanova M, Valkova E. Antimicrobial activity of Lactobacillus acidophilus against pathogenic and food spoilage microorganisms: A review. Agricultural Science and Technology. 2017;9(1):3-9.
- Wilson NL, Moneyham LD, Alexandrov AW. A Systematic Review of Probiotics as a Potential Intervention to Restore Gut Health in HIV Infection. Journal of the Association of Nurses in AIDS Care. 2013;24(2):98-111.
- Viljanen M, Pohjavuori E, Haahtela T, Korpela R, Kuitunen M, Sarnesto A, et al. Induction of inflammation as a possible mechanism of probiotic effect in atopic eczema–dermatitis syndrome. Journal of Allergy and Clinical Immunology. 2005;115(6):1254-9.
- Oak SJ, Jha R. The effects of probiotics in lactose intolerance: A systematic review. Critical Reviews in Food Science and Nutrition. 2018:1-9.
- Hungin APS, Mitchell CR, Whorwell P, Mulligan C, Cole O, Agréus L, et al. Systematic review: probiotics in the management of lower gastrointestinal symptoms – an updated evidence-based international consensus. Alimentary Pharmacology & Therapeutics. 2018;47(8):1054-70.
- Huang R, Hu J. Positive Effect of Probiotics on Constipation in Children: A Systematic Review and Meta-Analysis of Six Randomized Controlled Trials. Frontiers in Cellular and Infection Microbiology. 2017;7(153).
- Martínez-Martínez MI, Calabuig-Tolsá R, Cauli O. The effect of probiotics as a treatment for constipation in elderly people: A systematic review. Archives of Gerontology and Geriatrics. 2017;71:142-9.
- Coriat B J, Azuero O AJ, Gil Tamayo S, Rueda Rodríguez MC, Castañeda Cardona C, Rosselli D. Uso de probióticos en el síndrome de intestino irritable y enfermedad inflamatoria intestinal: una revisión de la literatura. Revista Colombiana de Gastroenterologia. 2017;32:141-9.
- Tangestani H, Emamat H, Ghalandari H, Shab-Bidar S. Whole grains, dietary fibers and the human gut microbiota: A systematic review of existing literature. Recent Pat Food Nutr Agric. 2020.
- Zhang Y, Zhang B, Dong L, Chang P. Potential of Omega-3 Polyunsaturated Fatty Acids in Managing Chemotherapy- or Radiotherapy-Related Intestinal Microbial Dysbiosis. Advances in Nutrition. 2018;10(1):133-47.
- Zhou S, Wang Y, Jacoby JJ, Jiang Y, Zhang Y, Yu LL. Effects of Medium- and Long-Chain Triacylglycerols on Lipid Metabolism and Gut Microbiota Composition in C57BL/6J Mice. Journal of Agricultural and Food Chemistry. 2017;65(31):6599-607.
- Rial SA, Karelis AD, Bergeron K-F, Mounier C. Gut Microbiota and Metabolic Health: The Potential Beneficial Effects of a Medium Chain Triglyceride Diet in Obese Individuals. Nutrients. 2016;8(5):281.
- de Souza EL, de Albuquerque TMR, dos Santos AS, Massa NML, de Brito Alves JL. Potential interactions among phenolic compounds and probiotics for mutual boosting of their health-promoting properties and food functionalities – A review. Critical Reviews in Food Science and Nutrition. 2018:1-15.
- Ayati Z, Amiri MS, Ramezani M, Delshad E, Sahebkar A, Emami SA. Phytochemistry, Traditional Uses and Pharmacological Profile of Rose Hip: A Review. Current pharmaceutical design. 2018;24(35):4101-24.
- Hu XY, Corp N, Quicke J, Lai L, Blondel C, Stuart B, et al. Rosa canina fruit (rosehip) for osteoarthritis: a cochrane review. Osteoarthritis and Cartilage. 2018;26:S344.
- Sweeney B, Vora M, Ulbricht C, Basch E. Evidence-Based Systematic Review of Dandelion (Taraxacum officinale) by Natural Standard Research Collaboration. Journal of Herbal Pharmacotherapy. 2005;5(1):79-93.
- Martinez M, Poirrier P, Chamy R, Prüfer D, Schulze-Gronover C, Jorquera L, et al. Taraxacum officinale and related species—An ethnopharmacological review and its potential as a commercial medicinal plant. Journal of Ethnopharmacology. 2015;169:244-62.
- Nikkhah Bodagh M, Maleki I, Hekmatdoost A. Ginger in gastrointestinal disorders: A systematic review of clinical trials. Food Science & Nutrition. 2019;7(1):96-108.
- Viljoen E, Visser J, Koen N, Musekiwa A. A systematic review and meta-analysis of the effect and safety of ginger in the treatment of pregnancy-associated nausea and vomiting. Nutr J. 2014;13:20.
- Ding M, Leach M, Bradley H. The effectiveness and safety of ginger for pregnancy-induced nausea and vomiting: A systematic review. Women and Birth. 2013;26(1):e26-e30.
- Viljoen E, Visser J, Koen N, Musekiwa A. A systematic review and meta-analysis of the effect and safety of ginger in the treatment of pregnancy-associated nausea and vomiting. Nutrition Journal. 2014;13(1):20.
- Auyeung KK, Han Q-B, Ko JK. Astragalus membranaceus: A Review of its Protection Against Inflammation and Gastrointestinal Cancers. The American Journal of Chinese Medicine. 2016;44(01):1-22.
- Christopher RW, Bernard r. Slippery Elm, its Biochemistry, and use as a Complementary and Alternative Treatment for Laryngeal Irritation. A J Physiol Biochem Pharmacol. 2012;1(1):17.
- Braun L. Slippery Elm. Journal of Complementary Medicine: CM, The. 2006;5(1):83.
- Amalraj A, Pius A, Gopi S, Gopi S. Biological activities of curcuminoids, other biomolecules from turmeric and their derivatives – A review. Journal of traditional and complementary medicine. 2017;7(2):205-33.
- Hosseini A, Hosseinzadeh H. Antidotal or protective effects of Curcuma longa (turmeric) and its active ingredient, curcumin, against natural and chemical toxicities: A review. Biomedicine & Pharmacotherapy. 2018;99:411-21.
- Maes M, Leunis J-C. Normalization of leaky gut in chronic fatigue syndrome (CFS) is accompanied by a clinical improvement: effects of age, duration of illness and the translocation of LPS from gram-negative bacteria. Neuro Endocrinology Lett. 2008;29(6):902-10.
- Sturniolo GC, Di Leo V, Ferronato A, D'Odorico A, D'Incà R. Zinc supplementation tightens “Leaky Gut” in Crohn's disease. Inflammatory Bowel Diseases. 2001;7(2):94-8.
- Clarke SF, Murphy EF, O'Sullivan O, Lucey AJ, Humphreys M, Hogan A, et al. Exercise and associated dietary extremes impact on gut microbial diversity. Gut. 2014;63(12):1913-20.
- Ortiz-Alvarez L, Xu H, Martinez-Tellez B. Influence of Exercise on the Human Gut Microbiota of Healthy Adults: A Systematic Review. Clin Transl Gastroenterol. 2020;11(2):e00126.
- ALLEN JM, MAILING LJ, NIEMIRO GM, MOORE R, COOK MD, WHITE BA, et al. Exercise Alters Gut Microbiota Composition and Function in Lean and Obese Humans. Medicine & Science in Sports & Exercise. 2018;50(4):747-57.
- Mailing LJ, Allen JM, Buford TW, Fields CJ, Woods JA. Exercise and the gut microbiome: a review of the evidence, potential mechanisms, and implications for human health. Exercise and sport sciences reviews. 2019;47(2):75-85.
- Ng QX, Soh AYS, Loke W, Venkatanarayanan N, Lim DY, Yeo W-S. Systematic review with meta-analysis: The association between post-traumatic stress disorder and irritable bowel syndrome. Journal of Gastroenterology and Hepatology. 2019;34(1):68-73.
- Galanakis M, Grammatikou T, Kalogridi S, Chrousos PG, Darviri C. Literature Review on Stress and Psychosocial Determinants of Irritable Bowel Syndrome. Psychology. 2016;Vol.07No.02:7.
- Jufang H, Gong H, Zhang C, Zhang Z, Wang W, Tian J. A systematic review of intervention effects of mindfulness-based stress reduction on irritable bowel syndrome. Chinese Mental Health Journal. 2018;32(2):106-11.
- Nichol AD, Holle MJ, An R. Glycemic impact of non-nutritive sweeteners: a systematic review and meta-analysis of randomized controlled trials. European Journal of Clinical Nutrition. 2018;72(6):796-804.
- Poulos SP. Reduced Calorie Sweetener Use Does Not Adversely Affect Gastrointestinal Health and Function. Journal of neurogastroenterology and motility. 2016;22(4):709-.
- Arrigoni E, Brouns F, Amado R. Human gut microbiota does not ferment erythritol. Br J Nutr. 2005;94(5):643-6.